

This article is based on a live interview between Debbie Denison, Merakoi Strategist, and Melanie Bahlke, Patient Expert in Obesity.
In the battle against obesity, new medications have emerged as powerful allies, offering hope to millions struggling with weight loss. However, as patient expert Melanie Bahlke reveals, these medications are just one piece of a much larger puzzle. Melanie, who leads the obesity surgery self-care association in Germany, paints a picture of obesity treatment that goes far beyond simply prescribing medication.
Melanie Bahlke is the Chairperson of Adipositaschirurgie Selbsthilfeverein Deutschland, focusing on obesity prevention and patient engagement, particularly for children and adolescents facing obesity challenges.
"For everyone (including physicians), this is a huge step," Melanie says, referring to the new obesity medications. "And for the patient, that's a new way to handle obesity." There's no doubt that these treatments have generated excitement and hope among patients, many of whom have struggled with weight loss for years.
However, Melanie is quick to point out a crucial limitation: "When you receive the medication, that's brilliant. But you have only changed your body and not your mind." In other words - while medications can be effective tools for weight loss, they don't address the psychological and lifestyle factors that contribute to obesity.
Both Melanie and Merakoi strategist Debbie Denison emphasize that medication alone is not enough to tackle obesity effectively. As Debbie notes, even the websites for these medications recommend combining treatment with diet and lifestyle changes. But Melanie goes further, advocating for a much more comprehensive program:
"The medication then can work better when patients have a good psychologist and nutritionist and somebody who will teach you to go out and have fun and make friendships."
Mental health support, nutrition guidance, and finding joy in activity - all these are the essential components for sustainable weight management.
Interestingly, Melanie challenges the use of the word "sport" (also meaning exercise), which can be intimidating for many living with obesity. Instead, she suggests focusing on "mobility":
"Mobility! I think there should be more mobility for your bones and for your muscles. The thing is we do not have a good build and core strength. I only have the muscles in the legs that can hold my weight."
This shift in perspective from "athletics" to "mobility" could be key in making physical activity more approachable and less daunting for those beginning their weight loss journey. It's a reminder that effective obesity treatment must be tailored to the specific needs and capabilities of each individual.
A recurring theme in Melanie's insights is the critical role of mindset and mental health in obesity treatment. She emphasizes that obesity often affects a person's entire outlook:
"So many people that are so affected from obesity that their whole mindset is confused. They have no structure and they need help."
This underscores the need for comprehensive support that goes beyond just physical interventions. Mental health resources, community support, and strategies for developing healthy habits are all crucial elements of a successful obesity treatment plan. Building supportive communities can play a vital role in managing chronic conditions like obesity.
Melanie challenges the traditional focus on weight as the primary measure of success in obesity treatment. She points out a crucial flaw in this approach:
"Instead of speaking about losing weight, we should speak about becoming healthy. When you are concentrated on your kilos, the circle starts again and again, and you lose motivation."
Obsessing over kilos lost can be counterproductive, potentially leading to cycles of frustration and demotivation. Instead, Melanie advocates for celebrating other indicators of progress, such as increased mobility, improved mental health, or enhanced quality of life. This views aligns with modern understanding of health, where factors beyond weight - such as metabolic health, cardiovascular fitness, and emotional well-being - define overall wellness.
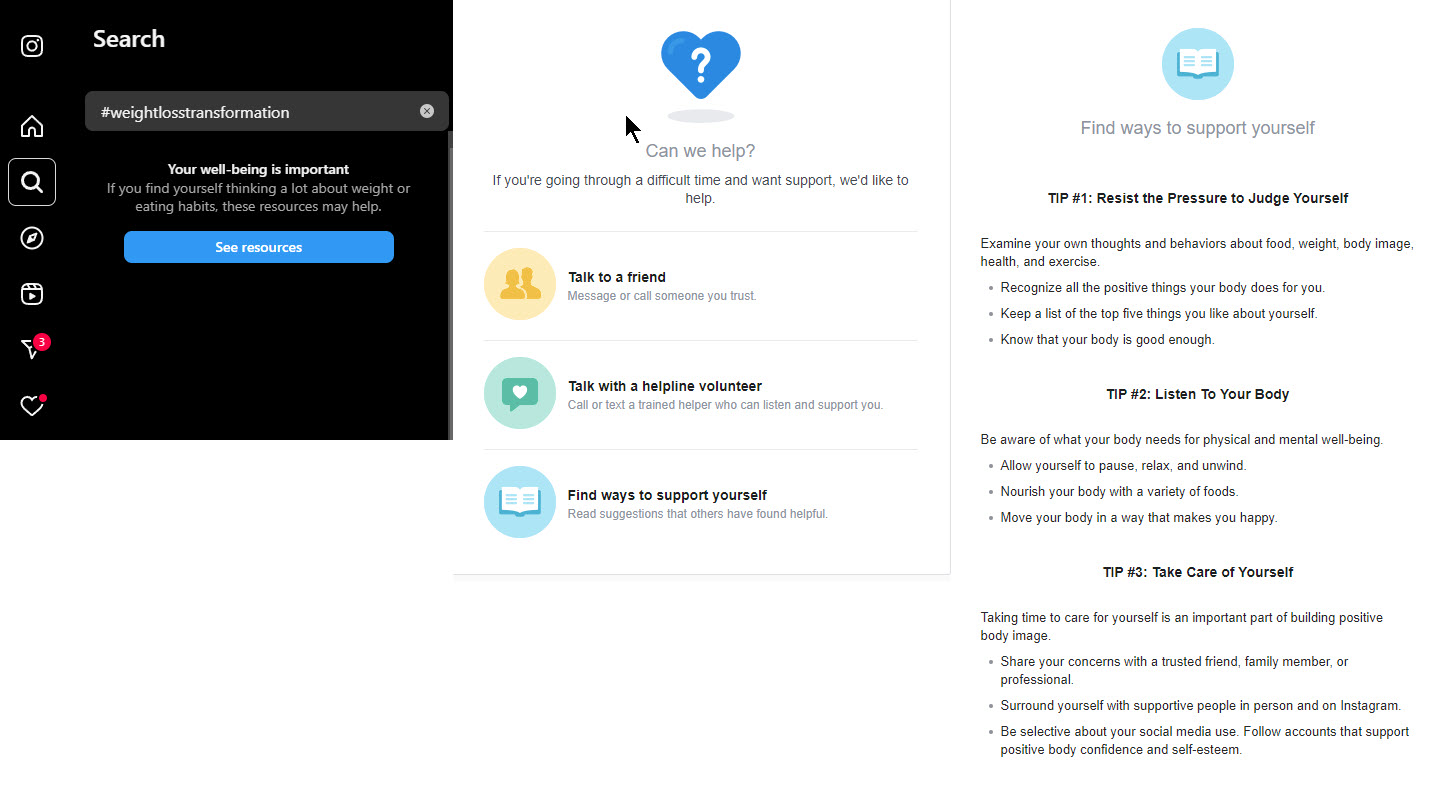
Digital health apps like Zoe and Noom have revolutionized weight management by focusing on behavioral psychology and lifestyle modifications. These apps use evidence-based techniques to help users reframe their relationship with food, develop healthier habits, and make sustainable changes.
While these digital solutions have proven effective for many users, they have yet to be fully integrated with breakthrough pharmacological treatments for obesity. The opportunity lies in connecting these two powerful interventions to create a seamless user experience.
Melanie highlighted the potential of this integration: "You can have digital apps in your pocket, in your hand, and that is something that is not visible. And you can have it all the time." For people with mobility limitations, traveling to frequent in-person appointments or classes can be difficult, uncomfortable, or even impossible. Yet, apps are just an arms length away.
By combining the behavioral support of digital apps with the physiological effects of medication, patients could benefit from a more comprehensive and personalized approach to weight management. This integration could help address the limitations of medication-only treatments by providing ongoing support, education, and motivation.
The challenge now is for pharmaceutical companies and digital health providers to collaborate and create solutions that seamlessly blend medication management with proven behavior change techniques.
Melanie proposes an intriguing model for initiating obesity treatment - a dedicated clinic or program where patients can start their journey:
"My wish is for a program, maybe two weeks, where you go to a clinic. They teach you, they give you the medication, and they provide knowledge about nutrition, mental health care, and all the other important aspects. It's not just about the medication - it's about learning how to manage your health."
This concept of a "kickstart" program that combines medication initiation with education and comprehensive support could be a game-changer in helping patients set themselves up for long-term success. It embodies the holistic approach that Melanie advocates for throughout her discussion.
Melanie’s message is straightforward: while new obesity medications offer valuable tools in weight management, they are not a silver bullet. To truly address this complex condition, we need a collaborative and innovative approach that brings together pharmaceutical innovations, digital health solutions, mental health support, and lifestyle interventions.
What stands out to me is the opportunity for cross-industry collaboration. Pharma, digital health, mental health, and even the fitness industry could create groundbreaking solutions by working together. Imagine a care platform that integrates medication management, psychological support, tailored mobility programs, and community engagement. This interview with Melanie has reinforced my belief that the next big breakthrough in obesity treatment won't come from a single sector, but from innovative partnerships that address the a spectrum of patient needs.
About Merakoi
At Merakoi, we're passionate about harnessing the power of mini-communities to bridge the information gap and empower patients to take control of their health journeys. By fostering ongoing collaboration between patients, healthcare providers, and pharma companies, we're creating a future where every patient has access to the knowledge and support they need to thrive.
Together, we can build a world where no patient is left in the dark, searching for answers. If this sounds like the kind of healthcare innovation you want to participate in, let's chat!

✕