

At merakoi, many of our projects begin with patient insights - on their treatment and disease journey, their experience in clinical studies or in clinic, their preferences and concerns when choosing or switching treatments. Patient journeys are inherently intricate and non-linear, each person’s experience with a disease is unique.
As projects progress from insights to solution co-design, we look to collaboratively address unmet needs with continuous input from patients, physicians and industry stakeholders. One of the key challenges when designing solutions is tailoring the experience to each person’s needs. Building mini-communities of patients and other stakeholders with shared experiences around a specific condition can provide valuable support and understanding.
Given the complexity of patient journeys, there is no one-size-fits-all approach that will work for everyone. Solution design often utilises a modular approach to deliver a personalised experience through self-segmentation. However, these modules need to incorporate behaviour change goals and the diverse needs of those adopting the solution. Failing to address this early on in the process leads to challenges in recruitment and retention, ultimately missing the opportunity to positively impact the lives of patients.
Let’s look into an example from an ongoing project to illustrate the complexity around segmenting patients for solution co-design. For this project, we are developing a digital therapeutic for people at moderate to high risk of stroke. We mapped hypertension across various disease pathways - from essential hypertension to comorbid conditions where hypertension is present and diseases where acute hypertensive episodes are likely.
Collaborating with a diverse mini-community representing potential conditions associated with hypertension, we focused primarily on the clinical journey while also incorporating areas where patients seek support and information outside the clinical setting. Utilising a train map analogy, we identified areas of moderate and high stroke risk to understand the points in the journey where a solution could benefit patients and their care teams.
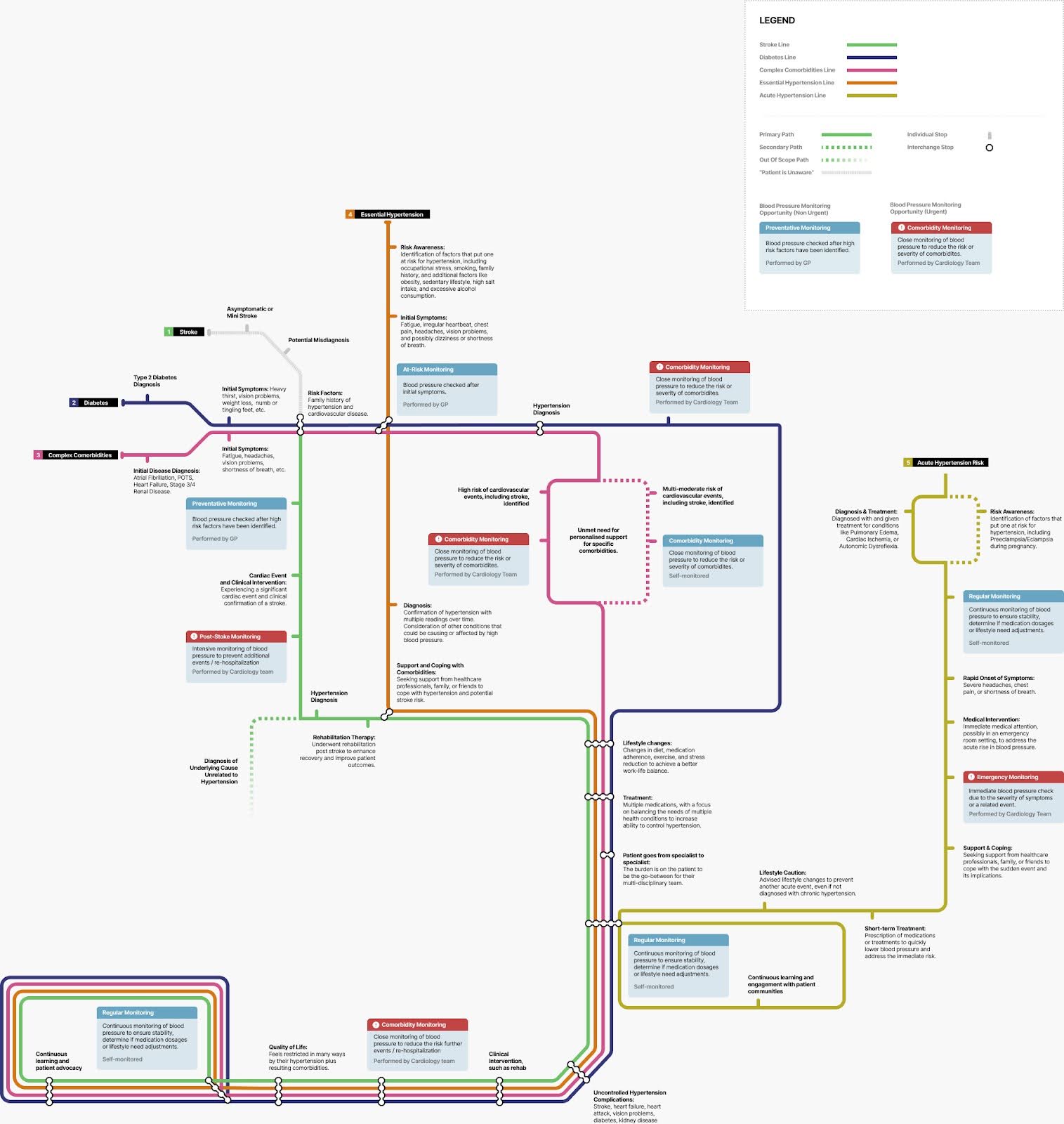
After mapping the patient journey, we moved to segmentation, to better understand those patients who were at the highest risk of stroke. We segmented by disease, number of comorbidities, access to specialist Centres of Excellence of Comprehensive Stroke Center, age, smoking status, treatment type and history of stroke. After aligning on the priority segments, we needed to understand their needs and concerns around disease management and uncontrolled hypertension.
Usage data or KPIs from existing digital solutions or patient support programmes would also need to be layered into the segmentation data. As you can see, this process can become quite overwhelming. Is there a simpler way to segment which could deliver equally effective results
It is widely accepted that people who have the knowledge, confidence and skills to manage their disease have better health outcomes than those who take a more passive approach. Highly activated patients living with long term conditions are more likely to engage in positive health behaviours and manage their disease, and their health, more effectively than those who have low levels of activation.
The Patient Activation Measure (PAM) is a framework is one of the foundations of personalised care adopted by healthcare systems in Germany, Denmark, Japan, the UK, Canada and others.
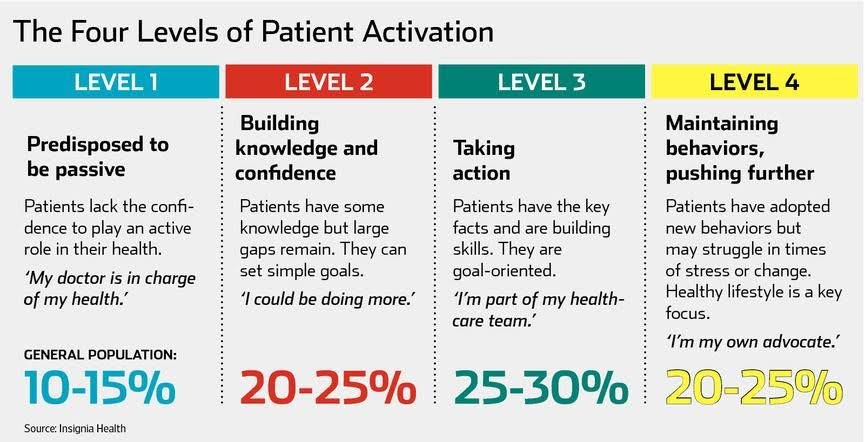
It’s easy to see how the PAM framework could be useful in moving patients from lower levels of activation to higher ones by empowering them with the knowledge and confidence they need to self-manage their disease. Roughly half of all people living with a disease could be in PAM levels 2 and 3, enabling you to address larger segments through your digital solution, PSP or digital therapeutic.
In a recent oncology project, where detailed patient data was lacking, we swiftly adapted by employing the PAM framework to create personas based on actual cancer patients. Engaging in sessions with mini-communities of cancer patients enabled us to gain valuable insights into the unique needs and challenges of people in each activation level. Insights were utilised to drive content planning and improve experience design , and create additional modules that had not been previously considered by the client team.
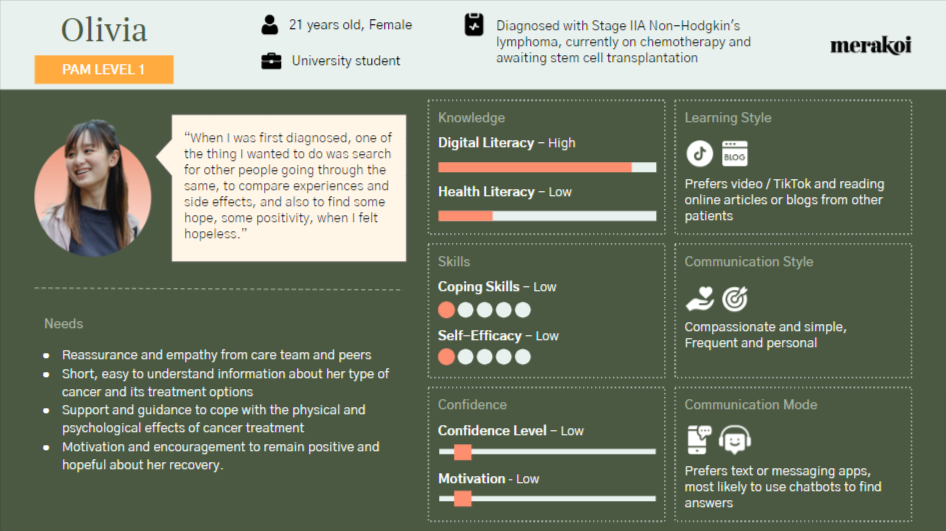
Olivia (not her real name) was a PAM level 1 patient living with Non-Hodgkin’s lymphoma. Everyone in the mini-community could empathise with Olivia - she was overwhelmed, disconnected from her disease management, had low levels of knowledge and few coping skills. People who are diagnosed with cancer typically start here, and it is very difficult to recruit or retain them onto digital solutions, apps, or patient support programmes in this stage.
During our sessions, we explored what Olivia would need in terms of resources, support / connection, appointment and side effect management. But we also looked at how that information could be presented in easy to digest formats that would help Olivia understand her disease at a time when she is ready to learn. We explored mental health concerns and how peers her own age who had been through a similar journey might be needed to help Olivia come to terms with her cancer and accept it.
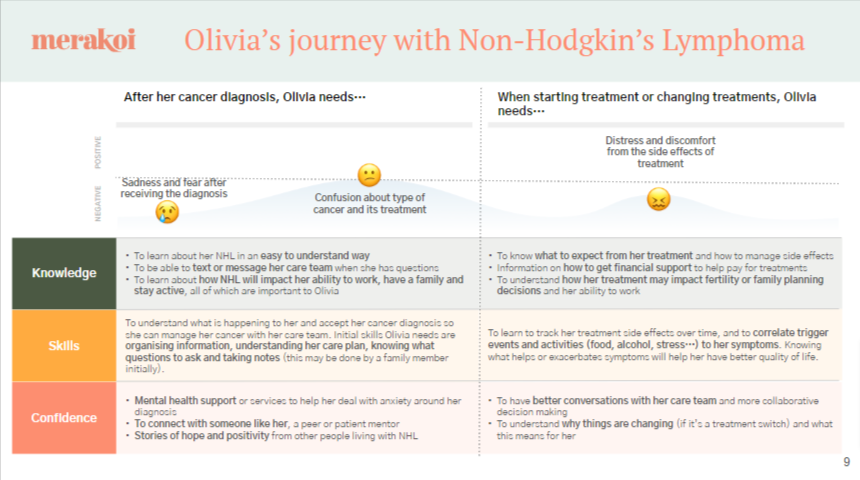
We repeated the process for our other personas in levels 2 to 4, taking the mini-community through each and asking them to walk in the shoes of each person to identify gaps and opportunities for the client team to meet the needs of each patient segment.
In this example, the cross-indication mini-community was able to walk in the shoes of other patient segments, providing valuable insights into their needs and challenges. Many members of the mini-community had been in similar situations throughout their own patient journeys or knew and interacted with peers in their communities who fit the specific segments and personas being explored. This shared experience allowed for a deeper understanding of the unique perspectives of each patient segment.
While the cross-indication community provided a strong foundation for understanding patient needs, including additional cohorts in the mini-community would allow for further exploration as the client moves from concept into solution design. These additional cohorts could include people with a specific tumour type, those on a specific treatment or type of treatment, those with an oncogene mutation, or those in a specific cancer stage.
By incorporating these specific cohorts, the team can gather targeted insights around the particular challenges the solution aims to address, ensuring a better fit for the intended patient population. For example, people living in rural areas who do not have access to a multidisciplinary team may struggle to share knowledge with physicians located in different clinics or hospitals. To address this challenge, the team could create a cohort that includes nurses from multiple specialisms involved in the patient's care, allowing them to understand the complexities patients face when being managed by both an oncologist and a nephrologist.
These additional cohorts would provide valuable feedback on the solution design, user experience, and content, enabling the team to make informed decisions and adjustments that improve the overall fit and effectiveness of the solution. By engaging with patients who closely match the target audience, the team can ensure that the final product addresses the specific needs and preferences of the intended users, ultimately leading to better adoption and outcomes.
Evidence shows that if we don’t address the levels of activation in people living with a disease, they are unlikely to benefit from the interventions we provide; they may not take their medications as prescribed, they may miss appointments, their conditions may progress faster, and they may develop additional comorbidities that could have been prevented. By focusing on activation as a driver for the solutions we create, we can provide a personalised experience that empowers them to better manage their health, and get better outcomes.
Ready to deliver a more personalised experience that meets the needs of patients? Contact us to learn how PAM plus mini-communities can elevate your patient interactions.
About Merakoi
Merakoi partners with health and life sciences companies to build mini-communities that guide product development through continuous user insights. Our network of patients/advocates and proprietary community platform enable engaging, longitudinal co-creation between users and developers. The result is human-centered solutions that resonate powerfully in the real world.

✕